Reminder: Updated version of CMS-1500 (02-12) instruction manual are released each July from public and private payers. Always refer to the specific instruction issued by your payer, clearinghouse, and/or vendor for further clarification of reporting requirements.
Online References:
Instructional Manual for New Form - CMS-1500 claim form completion instructions
New Claim Form Map - 837: (ASC X12) Health Care Claim Professional
Change Log from old version to new version
View the new CMS-1500 02/12 form by clicking here.

On June 17, 2013, The National Uniform Claim Committee (NUCC) Announced the approval of Version 02/12 1500 Health Claim Form (CMS-1500) that accommodates reporting needs of ICD-10. The Office of Management and Budget (OMB) has approved the CMS-1500 Claim Form under OMB Number 0938-1197.
During
its work, The NUCC was made aware by the health care industry of the changes
that were included in the revision to the CMS-1500 claim form:
1.
The addition of the scannable QR code on the left upper corner of the
claim form.
2.
The addition of an indicator in Item Number 21 to identify the version of the
diagnosis code set being report, eg., ICD-9 or ICD-10.
3. The expansion of the number for diagnosis
codes that can be reported in Item Number 21, which was increased from 4 to 12. FREQUENTLY ASKED QUESTIONS
1. Why was the 1500 Claim Form changed?
The 1500 Claim Form was revised to
accommodate reporting needs for ICD-10 and to align with requirements in
the Accredited Standards Committee X12 (ASC X12) Health Care Claim:
Professional (837P) Version 5010 Technical Report Type 3. During its work,
the NUCC was made aware by the health care industry of two priorities that
were included in the revisions to the 1500 Claim Form. The first was the
addition of an indicator in Item Number 21 to identify the version of the
diagnosis code set being report, i.e., ICD-9 or ICD-10. The need to
identify which version of the code set is being reported will be important
during the implementation period of ICD-10. The second priority was to
expand the number of diagnosis codes that can be reported in Item Number
21, which was increased from 4 to 12. Additional revisions will improve
the accuracy of the data reported, such as being able to identify the role
of the provider reported in Item Number 17 and the specific dates reported
in Item Number 14.
2. What are the specific changes that were made to the 1500 Claim Form?
2. What are the specific changes that were made to the 1500 Claim Form?
For a complete list of the changes from the current (05/08) version to the
revised (02/12) version, view the Change Log document posted on the NUCC’s
website under the “1500 Claim Form” tab here: Change
Log from old version to new version
3. What was the revision process that the 1500 Claim
Form went through?
The NUCC began revising the current 1500
Claim Form in 2009. The NUCC’s Data/1500 Subcommittee worked on how to
best revise the current form to accommodate various needs that were
identified and to better align with the Version 5010 837P electronic claim
transaction. Efforts were made to keep the changes minimal to limit the
amount of re-programming that would need to be done by the industry. The
NUCC’s work to revise the form included two public comment periods in
October 2009 and June 2011 to solicit feedback from the industry. All
comments received were reviewed and carefully considered when finalizing
the form. The revised version of the form was approved by the NUCC in
February 2012. Following the NUCC’s approval, the form was submitted to
the Centers for Medicare & Medicaid
(CMS) for their approval process with the Office of Management and
Budget (OMB). OMB approval of a form is required for it to be used in
government programs; in this case, government health care payers. As
part of their approval process, CMS conducted a 60-day public comment period
that was announced in the Federal Register in May 2012. CMS reviewed and
responded to the comments they received. The form was then submitted to
OMB for its approval and conducted an additional 30-day public comment
period in October 2012 that was also announced in the Federal Register.
The form was approved by OMB on June 11, 2013.
4. When do I have to start using the revised 1500 Claim Form?
Tentative Timeline for Implementing the Revised Form for Medicare Claims
• January 6 through March 31, 2014: Dual use period during which Medicare continues to receive and process paper claims submitted on the old CMS 1500 claim form (version 08/05).
• April 1, 2014: Medicare receives and processes paper claims submitted only on the revised CMS 1500 claim form (version 02/12).
Medicare anticipates implementing the revised CMS 1500 claim form (version 02/12) as follows:
• January 6, 2014: Medicare begins receiving and processing paper claims submitted on the revised CMS 1500 claim form (version 02/12). • January 6 through March 31, 2014: Dual use period during which Medicare continues to receive and process paper claims submitted on the old CMS 1500 claim form (version 08/05).
• April 1, 2014: Medicare receives and processes paper claims submitted only on the revised CMS 1500 claim form (version 02/12).
These dates are tentative and subject to change.View Medicare's website for full details and instructions about the new form. Sample New CMS-1500 Form here.
CMS-1500 form - version 02/12, will replace version 08/05, as announced by the National Uniform Transition Committee (NUCC). This revision allows providers to indicate whether they are using ICD-9 or ICD-10 codes, an important indicator as the transition in October 2014 approaches. This form allows additional codes (up to 12).
5. What is the symbol at the
top of the 1500 Claim Form?
The symbol is a Quick
Response code or “QR” code. If you take a picture of it with a smartphone
and the necessary app, it will take you to the NUCC website. Scanners
can be programmed to read the symbol and identify that the 1500 Claim Form
is the 02/12 version.
6. Why was Patient Status in Item Number 8 eliminated?
The data that was reported in this
field are not reported in the 837P, which is why the field was eliminated.
The NUCC intends to align reporting requirements of the paper 1500 Claim
Form with the electronic 837P transaction whenever possible.
7. Why was Other Insured’s Data of Birth, Sex in Item Number 9b
eliminated?
The data that was reported in this
field are not reported in the 837P, which is why the field was eliminated.
The NUCC intends to align reporting requirements of the paper 1500 Claim
Form with the electronic 837P transaction whenever possible.
8. Why was Employer’s Name or School in Item Number 9c eliminated?
The data that was reported in this
field are not reported in the 837P, which is why the field was eliminated.
The NUCC intends to align reporting requirements of the paper 1500 Claim
Form with the electronic 837P transaction whenever possible.
9. Why was Item Number 10d changed from Reserved for Local Use to
Claim Codes? Can I still report other data in this field?
The NUCC has limited this field for
the reporting of various claim codes, such as Condition Codes. Requests
for any additional codes that the industry would like to have reported
here should be brought to the NUCC. The need to report other data in this
field should also be brought to the NUCC, so the Committee can determine
the appropriate place to report that data. Requests for the NUCC can be submitted
at: info@nucc.org.
The data that was reported in this
field are not reported in the 837P, which is why the field was eliminated.
The NUCC intends to align reporting requirements of the paper 1500 Claim
Form with the electronic 837P transaction whenever possible.
11. Why Item Number 11b changed to Other Claim ID?
The NUCC received input on the need
to report Property and Casualty Claim Number. It was determined that a
broader need could be addressed by using the existing field and 3 creating
the ability to report a qualifier to indicate the type of number being reported. This
format allows for the flexibility to add additional qualifiers and types of
numbers in the future.
12. Why was a qualifier added to Item Number 14?
A qualifier was added to Item Number
14 in order to specifically identify which date is being reported in the
field.
13. Why was Item Number 15 changed to Other Date?
The NUCC received input that the
reporting of a date for Same or Similar Illness was not needed. There was
interest by the industry to be able to report other dates associated with
the claim. The ability to report a qualifier to indicate which date is being
reported was added. This format allows for the flexibility to add
additional qualifiers for other dates in the future.
A qualifier was added to Item Number
17 in order to specifically identify the role of the provider being
reported in the field.
Copyright 2013 American Medical Association
This document is published in cooperation with the National Uniform Claim Committee by the American Medical Association. Permission is granted to any individual to copy and distribute this material as long as the copyright statement is included.
15. Why was Item Number 19 changed from Reserved for Local Use to
Additional Claim Information? Can I still report other data in this field?
The NUCC renamed this field in an
effort limit the use of it as an open text field. Specific needs for
reporting data in this field should be brought to the NUCC, so the
Committee can determine the need and develop uniform instructions for the
reporting of the information. Requests for the NUCC can be submitted at:
info@nucc.org.
16. Why was a place added in Item Number 21 to report an indicator?
16. Why was a place added in Item Number 21 to report an indicator?
There will be a transition period
during the implementation of ICD-10 and an indicator is needed to identify
which codes are being reported on the claim; ICD-9 vs. ICD-10.
The NUCC received input from the
industry that the ability to report up to 12 diagnosis codes on a claim
was a priority. Refer to the picture above.
18. Why were the line labels in Item Number 21 changed from
numbers to letters?
The line labels are the diagnosis
pointers that are reported in 24E. Each service line (24) can point to up
to four diagnosis codes. Changing to letters was necessary because an
entry of “12” in 24E could be interpreted as both “1” and “2” or “12”.
In addition, there was not enough space in 24E to allow the reporting of
2-digit pointers and still accommodate up to four pointers. Refer to the picture above.
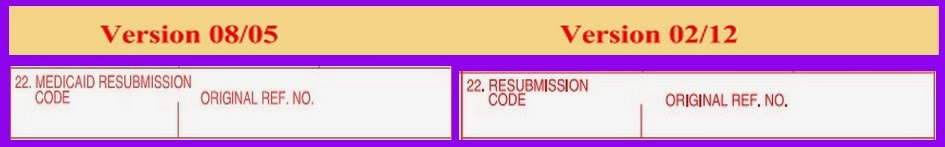
19. Why was “Medicaid” removed from the title of Item Number 22?
19. Why was “Medicaid” removed from the title of Item Number 22?
The data that was reported in this
field are not reported in the 837P, which is why the field was eliminated.
The NUCC intends to align reporting requirements of the paper 1500 Claim
Form with the electronic 837P transaction whenever possible.
21. Now that there are open fields, can they be used to report any
data, even though they are marked “Reserved for NUCC Use?”
No. These fields cannot be used to
report additional data. If there are needs to report additional data on
the 1500 Claim Form, the request should be brought to the NUCC, so the
Committee can determine the need and develop uniform instructions for
the reporting of the information. Requests for the NUCC can be submitted
at: info@nucc.org.
22. Why wasn’t “Pay-to Address” added to the 1500 Claim Form with
the revisions?
The NUCC had lengthy discussions
about the need to accommodate “Pay-to Address” on the 1500 Claim Form. The
final conclusion was that payers will use the address they have on file
for the provider to send payment. If the payer does not have the
provider’s address on file, they would want to contact them before sending
a payment to an address submitted on the form. Therefore, the NUCC
determined that it was unnecessary to accommodate “Pay-to Address” on the
form.
23. Do I have to use a 1500 Claim Form that is in red ink or can I
use a form that is copied or printed in black ink?
In order for the 1500 Claim Form to
be read by a scanner, the form must be in red ink. The red ink that is
specified for the form allows scanners to drop the form template during
the imaging of the paper. This “cleaner” image is easier and faster to
process with data capture automation such as ICR/OCR (Intelligent
Character Recognition/Optical Character Recognition) software. Your vendor
may choose not to process claim forms that are submitted in black ink.
24. My payer has given me different instructions for completing
certain Item Numbers on the 1500 Claim Form than what you have in your
instruction manual. Whose instructions should I follow?
The NUCC’s goal in developing the
1500 Claim Form Reference Instruction Manual is to help standardize
nationally the manner in which the 1500 Claim Form is completed. We do
recognize, however, that some payers will give their providers different instructions on
how to complete certain Item Numbers on the form. On the title page of
the instruction manual, it states: The NUCC has developed this
general instructions document for completing the 1500 Claim form. This document
is intended to be a guide for completing the 1500 Claim Form and
not definitive instructions for this purpose. Any user of this document
should refer to the most current federal, state, or other payer
instructions for specific requirements applicable to using the 1500 Claim
Form. Instruction Manual for New Form
25. My organization wants to insert its own specific instructions
into the NUCC Reference Instruction Manual. Can we do this?
No. Any payer-specific or other
organization-specific modifications to instructions must be maintained in
a separate document that references the NUCC Reference Instruction Manual.
26. Where can I find a crosswalk between the 02/12 1500 Claim Form
and the 837P?
A crosswalk between the 02/12 1500
Claim Form and the 837P is available on the NUCC website. The NUCC
Data Set, which is a more comprehensive mapping between the 837P and the
1500 Claim Form, is currently being updated for the 02/12 form. The updated
Data Set will be posted on the NUCC website once it is completed. New ClaimForm Map
CMS - 02/12 1500 Claim Form Starts in Jan 2014
The CMS-1500 Claim Form Revised to Support
CMS-1500 form - version 02/12, will replace version 08/05, as announced by the National Uniform Transition Committee (NUCC). This revision allows providers to indicate whether they are using ICD-9 or ICD-10 codes, an important indicator as the transition in October 2014 approaches. This form allows additional codes (up to 12).
About the NUCC
The 1500 Claim Form is maintained by the NUCC. The NUCC is a voluntary
organization of health care industry stakeholders representing providers,
payers, designated standards maintenance organizations, public health
organizations, and vendors. For more information on the 1500 Claim Form, visit
the NUCC website, www.nucc.org or email info@nucc.org.
For Medi-Cal CMS-1500 Claim Form Updates < - - - Click this link
For Medi-Cal CMS-1500 Claim Form Updates < - - - Click this link